|
|
Ladera Dental Implant Training - Dental Implant Education - Dr. Todd B. Engel, DDS - The Emergency Dental Implant
Released
on: October 6, 2009, 6:53 am The Emergency Implant An expert diagnostician will advise the very best treatment for a patient’s needs, regardless if the best course of treatment is a service that he or she routinely provides or not. In cases where the best treatment for the circumstances is not a treatment that is routinely performed in the office, then palliative treatment along with a referral to a specialist may be in order. Many more options are now available in the repertoire for restorative dentists placing dental implants. If the final result can be “blueprinted” prior to initiating treatment (and the clinician has the knowledge and ability to produce it), then some of the “afternoon emergency dilemmas” will appear a bit more straightforward, if not quite predictable. In this author’s opinion, there is no better feeling than consoling a distraught patient in an emergency situation, having the expertise to diagnose the emergency appropriately, and having the knowledge, confidence, and capability to produce a positive result for the patient. This article will attempt to illustrate a simplified method for an immediate implant placement, along with a guided tissue procedure, into a fresh extraction site. All of the standard “pre-procedural” diagnostic measures and conditions—with heavy emphasis on the patient’s health history—need to be considered and deemed acceptable before beginning treatment. These measures and conditions should include (but are not limited to):1 •
All pertinent clinical data In the following case report, a “prospective” new patient reported to the Ladera Ranch Implant Institute on a typical hectic afternoon in need of emergency treatment. Case
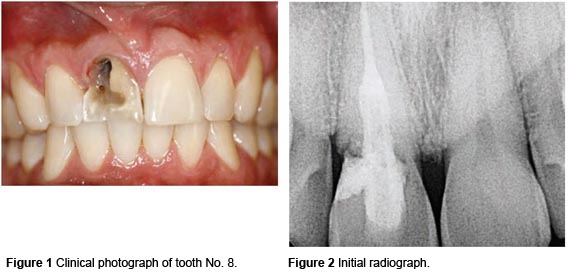
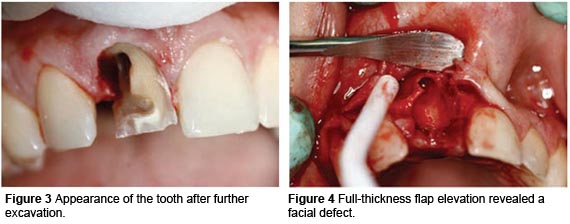
Report A complete dental examination was performed, as well as the review of his medica history. The medical history was unremarkable, and his dental condition was excellent with the exception of some localized, minimal tissue recession. The patient mentioned that he smoked more than a pack of tobacco per day, had no allergies, was not taking any prescribed medications, and that he was not under the care of a physician. During the intraoral evaluation (Figure 1 View Figure), the clinical crown was sacrificed after removal of the “loose filling.” Additional root caries was found extending well below bone level. The soft tissue surrounding the tooth was within normal limits. The preliminary x-ray (Figure 2 View Figure) revealed internal resorption, deep root caries, and biological width invasion. The culprit tooth had been previously treated with root canal therapy and a multi-surface composite filling. Aside from the patient’s complaint of the “filling feeling loose,” he had no other clinical symptoms. Treatment
Plan Communication is the first step to a successful blueprint. The patient was given the appropriate informed consent which included (but was not limited to) the proximity to the nasal floor and nasopalatine foramen, as well as possible pain, swelling, infection, damage to adjacent teeth, numbness (temporary or permanent), along with possible implant failure of unknown cause. Additionally (and, in the author’s opinion, a must for any implant surgery performed in the esthetic zone), informed consent was rendered for a potential need for a second periodontal surgical procedure, based on healing that may be less than ideal in the esthetic zone. Again, as with all smokers in need of treatment, a heavy emphasis was placed on the need for a healthy blood supply to reach the surgical site, and how the patient’s smoking would be a significant interference with respect to a successful outcome.2 Before beginning such a case, all provisional options and modalities must be considered and available before initiating surgery. This will help greatly in case of a potential shift in treatment plan mid-surgery. This is the stabilizer in most, if not all, successful anterior implant cases. Treatment
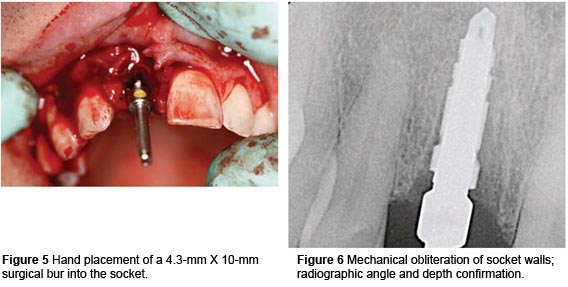
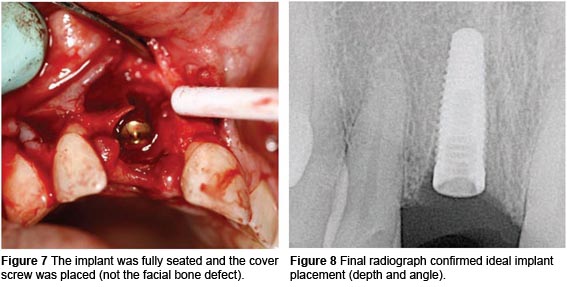
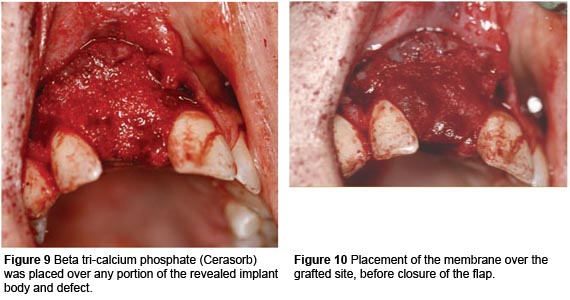
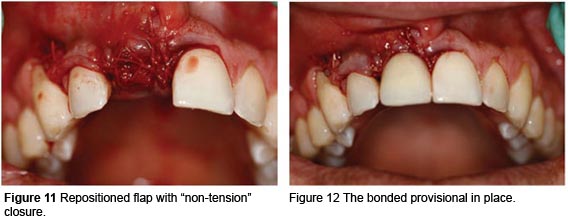
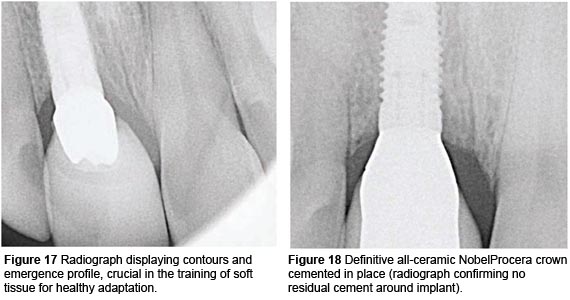
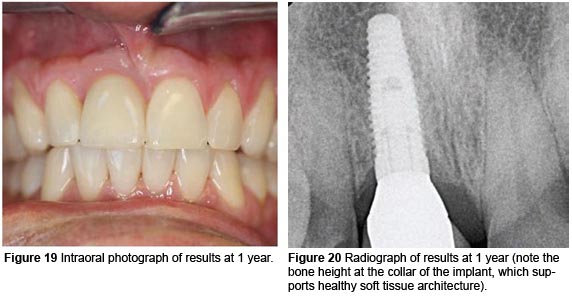
Protocol: Materials and Methods The patient was given a vestibular infiltration with one cartridge of lidocaine with epinephrine 1:50,000, along with supplemental infiltration on the palatal side of tooth No. 8. After complete loss of sensation was achieved, a periotome (Nobel Biocare, Yorba Linda, CA) was used to carefully separate the central incisor and its periodontal ligament (PDL) from the surrounding bony housing. This protocol is extremely important to ensure that the remaining boney housing is not jeopardized and/or fractured during the attempted tooth extraction. In cases such as this, further tooth breakage should be expected if one attempts to manually elevate or remove the remaining sacrificed tooth structure with forceps.4,5 After circumferential PDL detachment was accomplished, the central incisor was then atraumatically removed by simple elevation. This natural intact root would now serve as an ideal indicator of depth, width, and socket morphology, and would also confirm initial pre-surgical radiographic calculations. During further debridement and socket evaluation, a facial defect 3 mm in width and 3 mm in height was detected, necessitating the need for a full-thickness flap. The conservative flap extended both one tooth anteriorly and posteriorly, along with two vertical releasing incisions (Figure 4 View Figure), while keeping the base of the flap (vestibule) wider than the apex. This would maintain a healthy blood supply to the flap, prevent tissue necrosis, and would reduce the possibility of tearing or laceration when repositioning took place.6,7 Based on root morphology and size, a regular platform 4.3-mm X 10-mm NobelReplace™ Tapered Groovy implant (Nobel Biocare) was selected to complete the case. The surgical bur was then placed by hand directly into the socket to confirm a snug fit and also to confirm depth. The appropriate 4.3-mm X 10-mm surgical bur was then used to further obliterate the socket, gain apical advancement in virgin bone, and to create fresh bleeding internally. The implant was then placed into the fresh extraction socket, with emphasis placed on maintaining the desirable restorative angles and correct emergence profile as well as being respectful to all zones of safety (minimum of 2 mm) between the implant and adjacent natural teeth for an adequate and healthy blood supply.8 Based on the constriction toward the apical portion of the socket, a torque of 40 Ncm was achieved when the implant was placed in its final desired position. A cover screw was placed to seal off the opening of the implant in an effort to prevent any grafting debris from entering into the implant site (Figure 5 View Figure, Figure 6 View Figure, Figure 7 View Figure, Figure 8 View Figure). Next, before flap closure, the aforementioned facial defect was in need of repair. A pure-phase, beta tri-calcium phosphate, 150-µm to 500-µm particulate material, Cerasorb® (RIEMSER, Raleigh, North Carolina), was mixed with the patient’s own blood and placed directly onto the facial bone defect and exposed implant surface. All attempts were made to re-create the topography of the original bone pattern before any defect had occurred. Additionally, to protect and support the fresh clot and avoid any in-growth of unwanted epithelium into the graft itself, a bio-resorbable membrane, Epi-guide (RIEMSER), a bioresorbable synthetic membrane, was modified and placed directly over the Cerasorb graft material and beneath the tissue periosteum (Figure 9 View Figure and Figure 10 View Figure). The bio-resorbable membrane should remain a minimum of 1 mm away from the adjacent sulcus to prevent transmission of bacteria across the membrane surface from adjacent teeth. Although suitable torque was achieved to immediately load the implant, the author chose to delay loading because of the boney defect.9,10 Finally, and just before flap repositioning, a release of the underlying periosteum was indicated to ensure a relaxed flap closure and to avoid wound opening. The flap was repositioned with two horizontal mattress and four interrupted PTFE sutures (Osteogenics Biomedical Inc, Lubbock, TX) (Figure 11 View Figure). At this point, the temporization decision is key and quite critical to assist in healthy tissue healing and natural adaptation. A composite Maryland bridge provisional was fabricated chairside to complete this interim phase of treatment, in the effort of training and maintaining healthy, intact papilla by way of an ovate pontic design. Several try-ins were attempted before the final bonding to ensure that no contact was directly on the surgical site, at which time the temporary was adjusted out of occlusion and bonded into place (Figure 12 View Figure).11 The patient was prescribed amoxicillin 500 mg four times a day for 1 week, ibuprofen 800 mg three times a day for 4 days, and 0.12 chlorhexidine rinses three times a day for 1 week, and given a 10-day recall appointment. Before dismissal, the use of tobacco products was reviewed once again, and the patient was advised to refrain from smoking during the healing period. At the 10-day interval, the patient returned for a follow-up postoperative appointment. The bonded provisional restoration was removed for further evaluation of the surgical site and all sutures were removed. Ultimately, the provisional bridge was bonded back into place over the surgical site, and would remain in place throughout the remainder of the healing phase (Figure 13 View Figure). Based on the site evaluation and a short discussion with the patient, the first week proved to be successful. The patient was given a 4-month recall appointment for the restorative phase of treatment. At 4 months, the patient returned for the second phase, or restorative portion of treatment, which encompassed uncovering the implant fixture. Based on the author’s evaluation of healing after the 4-month period, an interproximal full-thickness flap was opted over a traditional “punch” technique to reveal the implant fixture for the implant-level impression. The rationale for this was to displace some of the healthy keratinized tissue from the palatal side of the implant, toward the facial aspect, as this would provide a more adequate biological seal and a more ideal esthetic result. This semi-lunar, full-thickness incision was initiated slightly palatal to the center of the ridge, while sparing the papilla interproximally (Figure 14 View Figure and Figure 15 View Figure). At this point, a transmucosal healing abutment was used to support, train, and maintain the repositioned flap for a more ideal result (Figure 16 View Figure). During the temporary phase, a well-designed provisional with ideally positioned proximal contact points is key, and will assist with overall papilla health (Figure 17 View Figure). Two weeks later, the patient returned for the definitive prosthesis, symptom-free. The all-ceramic NobelProcera™ crown (Nobel Biocare) was placed into position, and an x-ray was taken to confirm fit before cementation (Figure 18 View Figure). The NobelProcera crown was then cemented into place, the occlusal scheme was checked to make certain that the crown was solely in a light centric contact, and all parafunctional contacts were removed. The patient was very happy with his choice of treatment, as well as the final result (Figure 19 View Figure). Patient
Recall Conclusion
REFERENCES
2. Bain CA. Smoking and implant failure: benefits of a smoking cessation protocol. Int J Oral Maxillofac Implants. 1996;11(6):756-759. 3. Campelo LD, Camara JR. Flapless implant surgery: a 10-year clinical retrospective analysis. Int J Oral Maxillofac Implants. 2002; 17: 271-276. 4. Takayama H. Biomechanical considerations on osseointegrated implants. In: Osseointegration and Occlusal Rehabilitation. Hobo S, Ichida E, Garcia LT, eds. Chicago, Ill; Quintessence Int: 1989. 5. Cranin AN, Klein M, Simons AM. Soft tissue managing and grafting. Atlas of Oral Implantology. 2nd ed. St. Louis, Mo; Mosby Elsevier: 1992;94-170. 6. Sclar AG. Soft Tissue and Esthetic Considerations in Implant Therapy. Chicago, Ill; Quintessence Int: 2003;1-12, 43-162 7. Alfaro FH. Biology of bone grafting. Bone Grafting in Oral Implantology: Techniques and Clinical Applications. Chicago, Ill; Quintessence Int: 2006;9-26. 8. Cochran DL, Hermann JS, Schenk RK, et al. Biologic width around titanium implants. A histo-metric analysis of the implanto-gingival junction around unloaded and loaded nonsubmerged implants in the canine mandible. J Periodontal. 1997;68:186-198. 9. Khoury F, Antoun H, Missika P. Bone Augmentation in Oral Implantology. Chicago, Ill; Quintessence Int: 2007;1-28, 75-114, 341- 372. 10. Garg A. Bone: Biology, Harvesting, Grafting for Dental Implants. Rationale for Clinical Applications. Chicago, Ill; Quintessence Int: 2004;21-96. 11. Fabbri G. Recreating an aesthetic smile. Pract Proced Aesthet Dent. 2008;20(10): 593-598.
Private Practice
Dental
Implant Training
|
|



 Todd
B. Engel, DDS
Todd
B. Engel, DDS